[Article revised on 27 April 2020.]
Still today, many people with schizophrenia and their relatives, friends, and carers do not talk openly about the illness for fear of being misunderstood or stigmatized. This deplorable state of affairs can create the impression that the condition is very rare. It is in fact so common that most of us will know at least one person suffering with it. The lifetime prevalence of schizophrenia varies according to how the condition is defined, and is often quoted as 1 percent.
Schizophrenia can present at any age, but is rare in childhood and early adolescence. Most cases are diagnosed in late adolescence or early adulthood.
Unlike depressive and anxiety disorders, which are more common in women, schizophrenia affects men and women in more or less equal numbers. However, it tends to present at a younger age in men, and to affect them more severely. Why this should be remains unclear.
Schizophrenia exists in all cultures and ethnic groups, but, surprisingly, tends to have more favourable outcomes in traditional societies. This may be because tight-knit communities are more tolerant of mental illness and more supportive of their mentally ill. If true, it suggests that interpretations and attitudes can exert an important influence on the outcome of the illness.
The symptoms of schizophrenia are manifold, and present in such a variety of combinations and severities that it is impossible to describe a ‘typical’ case. In the short term, symptoms may wax and wane, with the sufferer experiencing both good days and bad days. In the longer term, the emphasis may shift from one group of symptoms to another, presenting different challenges for sufferer and carers.
The symptoms of schizophrenia are classically divided into three groups: positive symptoms, cognitive symptoms, and negative symptoms, as detailed in the table below.
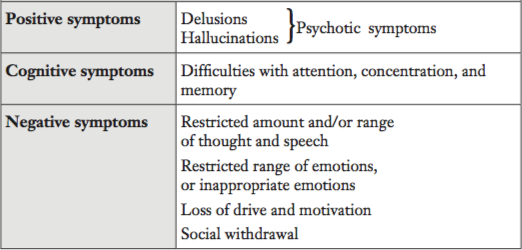
Positive symptoms consist of psychotic symptoms (hallucinations and delusions), which are usually as real to the sufferer as they are unreal to everyone else. Positive symptoms are considered to be the hallmark of schizophrenia, and tend to be most prominent in its early stages. They can be provoked or aggravated by stressful situations, such as leaving home for university, breaking off a relationship, or taking drugs (a form of biological, as opposed to psychological, stress).
Psychiatrists define a hallucination as ‘a sense perception that arises in the absence of an external stimulus’. Hallucinations involve hearing, seeing, smelling, tasting, or feeling things that are not actually there. In schizophrenia, the most common hallucinations are auditory, involving voices and sounds. Voices can either speak to the sufferer (second-person—‘you’—voices) or about him (third-person—‘he’—voices). Voices can be highly distressing, especially if they involve threats or abuse, or if they are loud and incessant. One might begin to experience something of this distress by turning on the radio and the television, both at the same time and at full volume, and then attempting to hold a normal conversation.
It should be noted that not all voices are distressing, and some, such as the voices of old acquaintances, dead ancestors, or guardian angels, can even be comforting or reassuring, and, at least in that much, may not be in need of ‘curing’.
Delusions are defined as ‘strongly held beliefs that are not amenable to logic or persuasion and that are out of keeping with their holder’s background or culture’. Although delusions need not be false, the process by which they are arrived at is usually bizarre and illogical. In schizophrenia, delusions are most often of being persecuted or controlled, although they can also follow other themes.
Positive symptoms correspond to everyman’s notion of ‘madness’, and people with prominent hallucinations or delusions often evoke fear and contempt. Such negative feelings are reinforced by selective reporting in the media of the rare headline tragedies involving people with (usually untreated) mental disorder. The reality is that the vast majority of schizophrenia sufferers are no more likely to pose a risk to others than the average person. On the other hand, they are far more likely to pose a risk to themselves. For instance, they may neglect their safety and personal care, or leave themselves open to emotional, sexual, or financial exploitation.
Cognitive symptoms involve problems with concentration and memory that can make it difficult to register and recall information, and to formulate and communicate thoughts. Cognitive symptoms are often detectable in the early, prodromal phase of schizophrenia before the onset of positive symptoms, and, though less manifest than positive symptoms, can be just as distressing and disabling.
Whereas positive symptoms can be thought of as an excess or distortion of normal functions, negative symptoms can be thought of as a diminution or loss of normal functions. In some cases, negative symptoms dominate the clinical picture; in others, they are altogether absent. Compared with positive symptoms, negative symptoms tend to be more subtle and less noticeable, but also more persistent, and can perdure right through periods of remission, long after any positive symptoms have burnt out.
Negative symptoms are often misconstrued by the general public, and sometimes also by relatives and carers, as indolence or obstinacy, rather than as the manifestations of a mental disorder. For health professionals, they can be difficult to distinguish from symptoms of depression, or from some of the side-effects of antipsychotic drugs.
The course of schizophrenia can vary considerably from one person to another, but is often marked by a number of distinct phases. In the acute (‘initial and short-lasting’) phase, positive symptoms come to the fore, while any cognitive and negative symptoms that may already be present sink into the background. The sufferer typically reaches a crisis point at which he comes into contact with mental health services. An antipsychotic drug is started and the acute phase resolves, even though residual positive symptoms may remain.
In some cases, the acute phase is preceded by a so-called prodromal phase lasting for anything from days to years and consisting of subtle and non-specific abnormalities or oddities that may be mistaken for depression or normal teenage behaviour.
As the acute phase remits, any cognitive and negative symptoms start to dominate the picture. This chronic (‘long-lasting’) phase, if it occurs, can last for a period of several months or even several years, and may be punctuated by relapses into a state resembling the acute phase. Such relapses are often caused by a sudden reduction or discontinuation of antipsychotic medication, substance misuse, or a stressful life event, although in many cases there is no identifiable trigger.
Complete recovery from schizophrenia is possible, but most often the illness runs a protracted course punctuated by episodes of relapse and remission. Overall, the life expectancy of people with schizophrenia is reduced by about 8-10 years compared to average, but this gap is narrowing owing to better standards of physical care. Perhaps surprisingly, the leading cause of death in schizophrenia is cardiovascular disease. Other important causes of death include accidents, drug overdoses, and suicide. The suicide rate is of the order of 5 percent, although rates of attempted suicide and self-harm are considerably higher.
Febrile illnesses such as malaria had been observed to temper psychotic symptoms, and in the early 20th century ‘fever therapy’ became a standard treatment for schizophrenia. Psychiatrists attempted to induce fevers in their patients, sometimes by means of injections of sulphur or oil. Other common but questionable treatments included sleep therapy, gas therapy, electroconvulsive therapy, and prefrontal leucotomy (lobotomy), which involved severing the part of the brain that processes emotions. Sadly, many such ‘treatments’ aimed more at controlling disturbed behaviour than at curing illness or alleviating suffering. In some countries, such as Germany during the Nazi era, the belief that schizophrenia resulted from a ‘hereditary defect’ led to atrocious acts of forced sterilization and genocide. The first antipsychotic drug, chlorpromazine, first became available in the 1950s. Although far from perfect, it opened up an era of hope and promise for people with schizophrenia.
Neurotransmitters are chemical messengers released by brain cells to communicate with one another and relay signals. Once released, neurotransmitters bind to specific receptors on target brain cells, causing them to react. According to the so-called dopamine hypothesis of schizophrenia, positive symptoms are produced by an increase in the neurotransmitter dopamine in a part of the brain called the mesolimbic tract. Support for the dopamine hypothesis comes, in the main, from two observations: (1) drugs such as amphetamines and cannabis that increase the level of dopamine in the mesolimbic tract can exacerbate the positive symptoms of schizophrenia or even induce a schizophrenia-like psychosis; and (2) antipsychotic drugs that are effective in the treatment of positive symptoms block the effects of increased dopamine in the mesolimbic tract. According to the dopamine hypothesis, the negative symptoms of schizophrenia result from a decrease in dopamine in another part of the brain called the mesocortical tract.
The dopamine hypothesis has supplied researchers with a basic model of schizophrenia, but says little about the actual cause of the changes in dopamine levels, and can by no means account for all the subtleties and complexities of the illness or its treatment. More recent research has implicated a number of other neurotransmitters such as glutamate and serotonin, although their precise roles remain unclear. It may be that altered levels of dopamine and other neurotransmitters are interrelated, once again raising the age-old problem of the chicken and the egg.
The dopamine hypothesis submits that antipsychotic drugs are effective in the treatment of positive symptoms because they block the action of dopamine in the mesolimbic tract. Unfortunately, they also block the action of dopamine in other brain tracts, commonly leading to a number of unpleasant side-effects such as negative symptoms, disturbances of voluntary muscle function, loss of libido, and erectile dysfunction. Antipsychotic drugs also interfere with neurotransmitters other than dopamine, which can result in further side-effects, first among which sedation and weight gain.
Still, antipsychotics remain the primary treatment for schizophrenia, although psychosocial interventions such as patient and family education, self-help groups, illness self-management, social and vocational skills training, and cognitive-behavioural therapy can all play an important role in reducing symptoms and preventing relapse and re-hospitalization.
Critics of antipsychotic drugs claim that there is nothing specifically ‘anti-psychotic’ about them, and that they are no more than a form of chemical control, or ‘chemical straightjacket’. They highlight that, before being rebranded as ‘antipsychotics’, the drugs used to be referred to as ‘neuroleptics’ (a portemanteau coined from the Greek for ‘nerve seizure’) or ‘major tranquillizers’. Physician Henri Laborit (1914-1995) who first trialled chlorpromazine himself described its effect as one of ‘artificial hibernation’.
Today, antipsychotic drugs are used not only in the treatment of psychosis, but also, in many cases, in the treatment or management of bipolar disorder, depression, dementia, insomnia, obsessive-compulsive disorder, post-traumatic stress disorder, personality disorder, and autism, among others—suggesting that any effect that they exert is far from targeted.
More specifically, some critics argue that discontinuation-relapse studies overstate the effectiveness of antipsychotic drugs, not least because the drugs sensitize the brain. This means that their discontinuation, especially if sudden, can leave the brain in ‘over-drive’ and thereby precipitate a relapse. The critics cite, among others, a 20-year longitudinal study led by psychologist Martin Harrow at the University of Illinois which found that longer-term antipsychotic treatment is associated with lower rates of recovery.
Last but not least, critics point out the obvious, which is that antipsychotic drugs often lead to unpleasant and restrictive side-effects, and significantly increase the risk of premature death.
Pioneered in Western Lapland, Finland, the innovative Open Dialogue approach to the management of a mental health crisis, including acute schizophrenia, de-emphasizes antipsychotic drugs. Instead, it focuses on immediate intervention to encourage the person and his family and wider network to come together and talk to one another, in part so that the person may find the words with which to express and lend meaning to his distress. Further studies are planned, but early indications are that the Open Dialogue approach can secure much better treatment outcomes while markedly reducing the use of antipsychotic drugs.
In 1949, neurologist Egas Moniz (1874-1955) received a Nobel Prize for his discovery of ‘the therapeutic value of leucotomy in certain psychoses’. Today, prefrontal leucotomy is derided as a barbaric treatment from a much darker age, and it is to be hoped that, one day, so too might antipsychotic drugs.
Neel Burton is author of the The Meaning of Madness and other books.